Good Killer Cells
Chemotherapy, radiotherapy or surgery – these are the three common forms of cancer therapy. The lymphoma specialists at University Hospital Essen are investigating the possibility of a different approach.
By Katrin Koster
Aggressive lymphomas – colloquially known as cancers of the lymph nodes – are the fifth most common cause of death from cancer in Germany. Can their treatment be improved via cellular immunotherapy? This is a possibility Prof. Dr Christian Reinhardt and his team are investigating at the Department of Hematology and Stem Cell Transplantation. In addition, they are developing further interdisciplinary therapeutic concepts and new procedures.
How, in a few words, does this novel immunotherapy work? ‘We’re speaking here about living drugs that dock specifically onto the cancer cells and act against them as killer cells,’ answers Christian Reinhardt, professor for internal medicine (hematology). The approach involves extracting T cells (T lymphocytes) from cancer patients, similar to a blood donation, and genetically modifying them on an individual basis: In the lab, they are given a surface molecule that later binds to lymphoma cells in the body, the so-called chimeric antigen receptors (CAR). This enables the genetically modified T cells to kill off the lymphoma cells in the body of the cancer patient.
The complex procedure takes two to five weeks, depending on how much time passes between extration and reinfusion. The method is still quite complex and, at around 300,000 euros per treatment, rather expensive. It is stillnot always covered by the health insurance schemes, but the positive results speak for themselves, and the processes will be refined further in the coming years. At present, these CAR T cells are used particularly for lymphomas, myelomas, and acute leukemias. ‘Together with the teams from the Department of Internal Medicine (cancer research) and the Department of Dermatology, we conduct clinical trials to analyse whether cellular immunotherapies could later also be used to treat solid tumours, such as lung cancer or melanomas,’ reports the doctor.
Reinhardt wants to help even more people suffering from cancer – of the lymph nodes, the tonsils, and the spleen, for example. The 46-year-old is therefore in the process of expanding the lymphoma department at the University Hospital Essen (UK Essen) and recruiting even more experts.
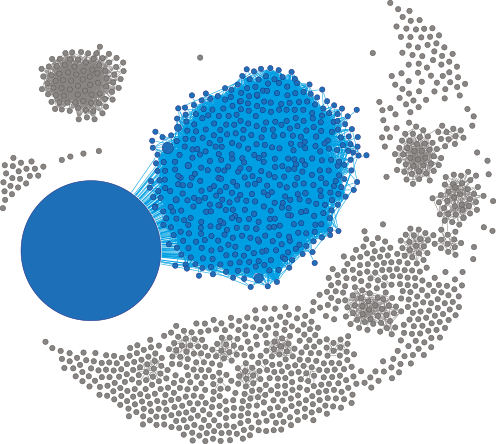
B cells are the body’s antibody factories. Every B cell formed carries an individual sequence of the B cell receptor (BCR), which it shares only with its progeny formed by cell division. Since all cells in a malignant lymphoma are derived from a single degenerate cell, all tumour cells consequently carry the same BCR sequence. The illustration shows the BCR repertoire of a lymphoma of this kind. Every circle stands for a number of cells with an identical BCR – the larger the circle, the more cells that carry the same receptor. The large blue circle represents a dominant population of cells with an identical BCR sequence. Thus, a single cell has expanded dramatically here, suggesting a malignant process. Also coloured blue are individual sequences that, although not identical, are so similar to the tumour sequence that they belong to the cancer population. The grey circles also stand for individual BCR sequences. They therefore symbolise healthy cells.
»We’re speaking here about living drugs that dock specifically onto the cancer cells and act against them as killer cells.«
Prof. Dr. Christian Reinhardt

CLINIC AND LABORATORIES
What remains particularly challenging is that tumours continue to develop: they do not stand still in their evolution and are very heterogeneous.
It helps to combine experience from the clinic and the laboratory. The team here at the West German Cancer Centre (WTZ) includes numerous dedicated minds: 50 doctors work with the nursing staff on the wards, 15 employees work in the research laboratory, up to 15 work in the diagnostic laboratory, and around ten work in the clinical trials center.
One of the research groups has developed a new mouse model that can be used to understand the processes in human cells even better. ‘It enables us to determine with greater precision which lymphomas respond to which CAR Ts,’ says the doctor, describing the steps used to further characterise the chimeric antigen receptor cells. All this helps the researchers to develop individualized therapy approaches and generate preclinical data.
‘Our genetic perspective sets us apart from other hospitals. And even though we have been working on immunotherapy for years, our projects have received new attention since the 2018 Nobel Prize was awarded for the discovery of immune checkpoints.’ Since then, even more extensive research has been conducted on how the patient’s own immune system can be activated to fight against the tumour.
There are also other cancer therapies that can work without chemotherapy. One such therapy that is successful for various chronic and acute leukemias, for example, are certain tablets that do not have a DNA-damaging effect – meaning that they conserve normal tissue – and that intervene by intercepting critical intracellular signaling events in cancer cells. They are extending the chances of survival from months to years already today.
AWARD-WINNING
For his contribution to basic research to better understand cancer and develop new treatment options, Prof. Dr Christian Reinhardt has been awarded the German Cancer Prize 2023 in the Experimental Research category. The prize awarded by the German Cancer Society and the German Cancer Foundation is one of the most important awards in oncology and is endowed with 7,500 euros. It is awarded annually in four categories.
UNDERSTANDING CANCER CELLS
The search for such new chemical sustances that can be used to combat life-threatening cancers in a more targeted manner is also the task of a new project. It was launched just a few months ago and is receiving 19.4 million euros in funding from the state government of North Rhine-Westphalia. Under the acronym CANTAR (CANcer TARgeting), scientists are building up a unique network of experts from chemistry, biology, and medicine throughout Germany. The project is being led by the University of Cologne and will run until July 2026. Other participating institutions include the Universities of Duisburg-Essen, Dortmund, Düsseldorf, Aachen and Bonn, as well as the Max Planck Institute for Molecular Physiology and the German Center for Neurodegenerative Diseases.
If we identify the specific drivers of cancers, we can block them. In addition, we are interested in understanding how cancer cells can ward off an attack from the body’s own immune system,’ says Reinhardt, who directs the research on this topic at the Essen project location. Thus, the Department of Hematology and Stem Cell Transplantation and its partner organisations are taking their research in many directions – with the common goal of progressively reducing the use of chemotherapy.
TOP-NOTCH RESEARCH
Prof. Dr Christian Reinhardt is in charge of subprojects in three different CRCs: CRC 1430 Molecular Mechanisms of Cell State Transitions at UDE (spokesperson: Prof. Dr. Hemmo Meyer); as well as CRC 1399 Mechanisms of Drug Sensitivity and Resistance in Small Cell Lung Cancer; and CRC 1530 Elucidation and Targeting of Pathogenic Mechanisms in B cell malignancies. The two last-named CRCs are based at the University of Cologne; UDE professor Reinhardt serves as their vicespokesperson.
He also contributes his expertise to the Europe-wide consortium ERA PerMed, with partners from Austria, France and Italy, to find new therapies for a particular subtype of aggressive lymphoma. In addition, he is a member of the consortium InCa on lung cancer, funded by the Federal Ministry of Education and Research. Furthermore, Reinhardt is cospokesperson of the North Rhine-Westphalian network CANTAR, which is developing new active substances for the research and treatment of cancer.
Main image: Immunofluorescence staining can be used to visualise the interaction of signalling proteins in a lymphoma (here from a mouse): DNA is dyed blue, making it possible to identify individual cell nuclei. By way of a special biochemical method (proximity ligation assay), red staining occurs when two specific signal proteins come together in close proximity (up to 40 nanometres) and apparently interact. | © AG Reinhardt