Please Treat Unequally
Height: just under 1.80 meters; weight: approximately 85 kilograms. One X and one Y chromosome. This has been more or less accepted as the norm in medical research – until now. Prof. Dr Anke Hinney is about to change that.
By Jennifer Meina
Biologically, women are not simply smaller and lighter men. They generally have more adipose tissue, while men tend to be more muscular. Bone structure also differs between the two sexes. They experience pain differently. Their organs work at a different speed and have different weights and sizes. The hormonal setup of a woman is subject to lifelong fluctuations, whereas hormone levels in man are mainly stable with a slight decline in higher age. Despite all these well-established biological differences, men are still regarded as the norm in medical research – in diagnostics, in dosages of medications, and in treatment. Anke Hinney knows how dangerous the results of such biased research can be for patients. The head of the Molecular Genetics Research Division at the Department of Child and Adolescent Psychiatry, University Hospital Essen is professor for molecular genetics of obesity and eating disorders with a focus on gender-specific aspects.
‘If the disease manifests in the “wrong” sex, i.e. the non-standard one, this could not only result in poorer quality of treatment but can sometimes even have fatal consequences.’ It is well-known that the symptoms of a heart attack often manifest differently in men and women – women are more likely to experience nausea and stomach discomfort rather than chest pain and shortness of breath. Other diseases are not even considered as possible diagnosis when the ‘non-standard’ sex is affected. For example, about 40 per cent of women and 20 to 30 per cent of men are affected by osteoporosis in later life. Although the disease afflicts men less commonly, it is by no means as rare as generally assumed. Nevertheless, a femoral neck fracture or a vertebral body fracture is rarely associated with osteoporosis in men. Psychiatric disorders also show sex-specific differences. Eating disorders are much more common in women than in men. Within the field of somatic disease breast cancer presents as a sex-specific disease. Yet men can be affected as well. When they are, diagnosis often does not occur until a very late stage. After all, in contrast to women, men are not trained to regularly examine their breasts for lumps – and then, should they suspect the disease, are not likely to consult a gynaecologist for diagnosis.
»If the disease manifests in the “wrong” sex, i.e. the non-standard one, this could not only result in poorer quality of treatment but can sometimes even have fatal consequences.«

AVOIDING BLIND SPOTS
‘There are countless such examples,’ Hinney attests. ‘Therefore, we urgently call for re-examination – in society, for one thing, but especially also in research and medical practice.’ And things are starting to happen: ‘Gender Medicine’ (see box) has been offered as an elective at the UDE Faculty of Medicine since 2020. In addition, Prof. Dr Anke Hinney, Assistant Professor Dr Andrea Kindler-Röhrborn, and Prof. Dr Arzu Oezcelik have teamed up with the Essen College of Gender Research (EKfG) in an effort to support other scientists at the Faculty of Medicine and the University Hospital in taking sex-specific differences into account in new projects. ‘The aim is to avoid blind spots in research and to enhance the scientific quality of the results,’ says Hinney. Most researchers still only identify this blind spot by accident.
‘Many conduct their studies and then only review in the last step which data sets are from which sex – and are surprised when they see how different the results can be.’ There are now roughly 40 medical scientists and clinician scientists at the University Hospital Essen who are involved in sex-sensitive medicine and consciously include sex and gender aspects in their studies. It is often impossible to obtain data on women from earlier studies, due non-inclusion.
This gender data gap is not only considerable in medicine. Most products of daily life and their safety testing are traditionally oriented towards male needs. This may not be dangerous for women in the case of mobile phone design, but it is an entirely different situation when it comes to car crash tests or medications.
Medications, for example, were only tested on men for decades. That was well intentioned: the female cycle did not have to be taken into account; pregnancies could not be endangered. The inclusion of women in drug research requires the exclusion of pregnancy. ‘One problem is that drugs that did not work in men and were therefore discarded during testing might have worked in women,’ Hinney says. The biologist admits: by including women in the studies, things get more complicated. Because now twice as many test subjects are needed – or twice as many animals in the lab. But there is no alternative for her: ‘We don’t want distorted results, we want medicine that is based on objective data.’

BALANCED DISADVANTAGE
Hinney had her moment of aha while investigating genetic mechanisms for eating disorders. Some of the genetic mechanisms that regulate body weight are also responsible for eating disorders. ‘In a large-scale study, we found three gene loci relevant for both the development of anorexia nervosa and for weight regulation. When we subsequently analysed this in a sex-specific manner, it turned out that the genetic variants at one of these gene loci are relevant for weight regulation predominantly in women.’ That, says Hinney, is particularly fascinating, because anorexia nervosa is diagnosed significantly more often in women than in men. It is still unclear how, precisely, the mechanism works and how the finding can be used for an improved treatment.
Andrea Kindler-Röhrborn of the Institute of Pathology made similar discoveries in a study in which rats were administered a carcinogenic substance. Strikingly, the male animals developed tumours significantly more often; and if any did develop in female animals, it was only after twice as much time had passed. She is currently investigating this phenomenon by identifying gene loci involved both in the development of tumors and the molecular mechanisms that may prevent this. Previous research already provides two conclusions: (a) There are certain tumour resistance genes in the body. If these are located on X chromosomes and carry variants that lead to a loss of function on one X chromosome, the loss in women can be compensated for by the second X chromosome; but not in men who only have one X chromosome. This mechanism means that certain hereditary diseases are much less common in women than in men. (b) The sex hormone estrogen, which is found in much higher concentrations in women than in men, could have a protective effect – as has already been demonstrated for the heart, circulatory system, and blood vessels. Women are less likely to suffer from these specific diseases before menopause.
It was also established for a long time that men were about 1.8 times more likely to develop different forms of cancer – the analyses did not include the sexual organs. ‘Men are biologically worse off than women – and then there is often an unhealthier lifestyle,’ explains Kindler-Röhrborn. More alcohol consumption, less exercise, or an unhealthier diet can all promote the development of tumors. The role of sex-specific gene variants and hormones – the ‘big players in gender differences,’ as the two scientists call it – is now a proven additional risk. In the future, the results of this research are to be implemented in gender-adapted preventive medicine.
Arzu Oezcelik, professor for visceral organ transplantation, has identified important sex differences in her work as well. For example, women are at a double disadvantage in liver transplantation: for one thing, donor organs are allocated according to the MELD score (model for end-stage liver disease). This system indicates the severity of a liver disease and is calculated on the basis of particular laboratory variables that are different for men and women. However, no distinction is made between the sexes. In concrete terms, this means that women often appear to be healthier on paper, this not being the case in medical terms. Thus, they receive a lower rank on the transplant list. In addition, most donor organs come from male donors – and are sometimes difficult to fit into the smaller and more slender bodies of women. And even if they do, women are more likely than men to reject these organs. To prevent this, immune suppressants will have to be dosed on a sex-specific basis in the future.
»If the algorithm is only trained with data collected from male subjects, the computer can only derive a corresponding diagnosis and treatment.«

FROM MINOR ADJUSTMENTS TO MAJOR CHAGES
The fact that not only humans need to be re-trained to consider the sex and gender based differences is also shown by the experience with artificial intelligence, which is playing an increasingly important role in medicine. Scientists are already working intensively with UDE’s own Institute for Artificial Intelligence in Medicine (IKIM). But here too, data gaps and gender bias can have an unfavourable impact on research, on development, and consequently on patient care. In other words, algorithms also have to account for diversity. ‘If the algorithm is only trained with data collected from male subjects, the computer can only derive a corresponding diagnosis and treament,’ says Dr Anke Diehl, Chief Transformation Officer at the University Medicine Essen and lead manager of the KI.NRW-Flagshipproject SmartHospital.NRW, making it clear that analogue mistakes must not be repeated in the digital world.
The scientists have a clear goal: improving treatment for all sexes, according to their specific needs. It is also important to stress that women and men have more similarities than differences. ‘We must identify, study, and treat the various forms of a singular disease, but it’s usually just a matter of minor accommodations like an adjusted drug dosage. Sometimes, however, we need entirely new treatments,’ stresses Hinney.
Another group must also be included: non-binary or transgender people. Which treatments are most suited for diseases in these individuals? These questions have come up more and more in recent years. The difficulty answering them lies in the fact that it is a very small group of individuals for which there is only very little data. ‘In the future, however,’ says Hinney, ‘the topic will certainly also feature more prominently in research and treatment.’
GENDER MEDICINE IS AN OUTDATED TERM
Although ‘gender medicine’ is currently on everyone’s lips, the term ‘sex- and gender-sensitive medicine’ is more appropriate. This is because the word ‘gender’ refers to social differences, whereas the word ‘sex’ refers to biological differences – biomedical research focuses on the latter. Awareness is growing: At the end of 2022, the ‘Netzwerk Geschlechtersensible Medizin NRW’ (North Rhine-Westphalia network for sex- and gender-sensitive medicine) was founded by the Faculties of Medicine at the Universities of Aachen, Bielefeld, Bochum, Duisburg-Essen, Düsseldorf, Cologne, Münster and Witten/Herdecke.
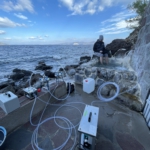
Main image: © Annika Huskamp