A Virus Against Cancer
What if a patient’s own immune system could fight a primary tumour and metastasis – both at once – with a virus sounding the attack? That is the vision of the start-up Abalos Therapeutics GmbH.
By Birte Vierjahn
Tackling cancer with viruses might at first sound like fighting fire with fire. Yet it is a promising idea, and in recent years many approaches have relied on oncolytic viruses that directly destroy cancer cells. However, there is a problem: to do this you have to infect each individual tumour cell with the virus, and this is pretty much impossible. So Prof. Dr Karl Lang (UDE) and his brother Philipp (professor at Heinrich Heine University Düsseldorf, HHU) had a different idea when they founded Abalos Therapeutics GmbH in October 2019 (see box).
They want to make cancer patients’ immune systems fight the tumour cells for them. Like neon coloured adhesive labels, specially designed viruses mark out the tumour cells. The Langs learned the principles of this from an eminent authority: as postdocs they both worked in the laboratory of Rolf Zinkernagel, who received the Nobel Prize in Medicine in 1973. Together with an Australian colleague he had proven how the immune system recognises virus-ridden cells.
This finding is the basis for Abalos’ therapeutic approach: the start-up, which cooperates with researchers from UDE and HHU, works with the lymphocytic choriomeningitis virus, or LCMV, an arenavirus that has already been studied in depth. Arenaviruses are known to replicate for preference in tumour cells and therefore activate both types of the human immune system: the innate, which acts immediately but quite arbitrarily to tackle anything that is not particular to the body, and the acquired immune system which takes longer to form, but then addresses the individual enemy with customised weaponry. In addition, LCMV replicates rapidly in tumour cells and remains inside them for a long time. This is important for the subsequent process: basically, cells that are attacked by viruses react by presenting fragments (peptides) of the intruders on their surface and sending out immune activating molecules (cytokines). This is the cells’ alarm call to the immune system: ‘I’m infected, and this is the pathogen!’ Specialist immune cells – monocytes and cytotoxic CD8+ T cells – recognise the signals and destroy the affected cells together with their potentially harmful content. In a simple infection such as a cold virus, the destruction of the body’s own cells is collateral damage – the real objective are the viruses that have proliferated inside them. By contrast, Abalos’ virotherapy aims to kill the tumour cells, and the viruses are highly-specialised target markers, a means to an end.
43 MILLION EUROS FOR VIRUS THERAPY
Prof. Dr Karl Lang, director of the Institute of Immunology (UDE), and his brother Philipp (Heinrich Heine University Düsseldorf) founded Abalos Therapeutics GmbH in October 2019. The Düsseldorf-based start-up researches specific arenaviruses, which activate the immune cells of cancer patients and can help target tumours precisely: in this way, the body’s own defence system fights and destroys the out-of-control cells. The start-up has managed to attract a total of 43 million euros in two financing rounds – e.g. from the Boehringer Ingelheim Venture Fund and the financial investor Seventure Partners, the venture capital fund Coparion and the NRW Bank. Clinical trials into virus therapy are due to start in 2024.
SPEEDING UP EVOLUTION
In order for LCMV to fulfil its role without giving rise to undesirable side-effects, it is customised. To do this, Abalos uses a ‘Fast Evolution’ platform – to speed up evolution, as the name suggests. The researchers allowed arenaviruses to grow in parallel in various tumour cells and observed the naturally occurring mutations. And in the same way as when cultivating apples, we propagate those that are especially tasty, easy to grow and robust, the eighteen-person team at Abalos looked for and aimed to combine three characteristics. In particular, in the over 100 mutations they observed if
1. the virus penetrates tumour cells efficiently,
2. it proliferates rapidly inside the cells,
3. once there, it effectively activates the immune system.
A fourth criterion, patient safety, was ensured by weakening the viruses’ capacity to infect liver cells. Also for safety reasons, their life-cycle end is programmed: although the viruses can withstand the body’s defence mechanisms for long enough, once their job is done, the CD8+ T cells make short work of the little helpers. ‘All the criteria together have led to a very promising and safe virus candidate, with which we are now in preclinical studies,’ CEO Dr Marcus Kostka sums up.

LONE WOLVES AND TEAM PLAYERS
In 2024 Abalos wants to take its virus candidate into clinical trials. Best suited to such treatment are solid tumours, i.e. those accompanied by tissue growth – in contrast to leukaemia, for example. The viruses are administered intravenously and automatically identify the tumour cells, where they proliferate and trigger the body’s defences. They can either be used alone or in combination with other forms of therapy, for a synergistic effect. For instance, in Phase 2 of the planned clinical trials the Abalos team will combine its virus with checkpoint inhibitors: tumour cells develop their own defence mechanisms which prevent them being identified as dangerous and consequently destroyed. Checkpoint inhibitors are still very new drugs that block these cancer cells’ inherent protection – unfortunately, they do not work in every patient. ‘We hope that combination with our virus therapy will bring about a decisive breakthrough here,’ says Kostka.
If the clinical trials are also successful, Abalos’ viruses could make every tumour cell vulnerable – regardless whether they are in the primary tumour or far-off, perhaps not yet detectable metastases.
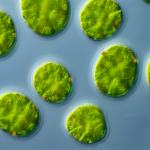
Main image: © Abalos Theropeutics GmbH